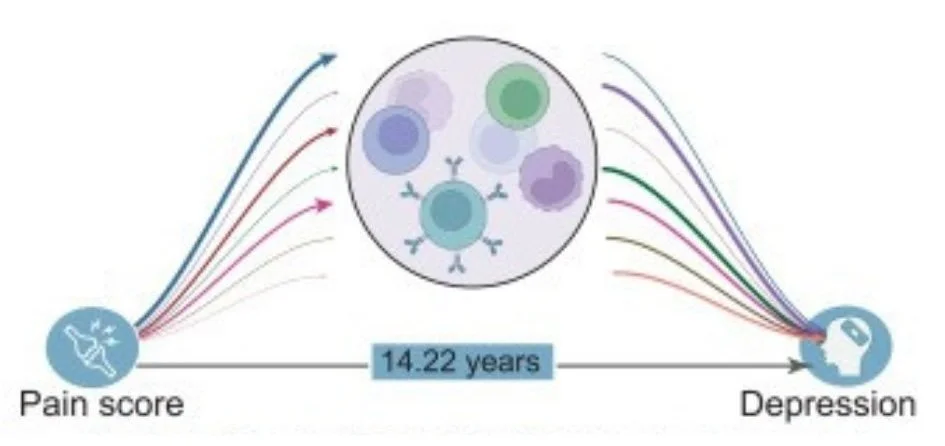
How Pain and Depression Are Connected: Insights from a 14-Year Study of 430,000+ People
A large study links pain in multiple body areas to much higher depression risk. Learn how inflammation and lifestyle matter.
Study: Inflammatory & Genetic Mechanisms Underlying the Cumulative Effect of Pain Conditions on Depression
Chronic pain is a daily reality for nearly 30% of people worldwide and is one of the top reasons for seeking healthcare. As a physician specializing in integrative pain management, I see every day how pain and mood are deeply connected. A newly published study of over 430,000 adults followed for 14 years offers powerful data on how pain—especially when it affects several body areas—can sharply increase the risk of depression.
These findings are not just statistics; they offer practical insights for anyone living with pain or supporting someone who is. Below, I cover a few of the main findings I found interesting.
The Main Findings: More Pain Sites, Higher Depression Risk
The study analyzed pain across eight body sites (like head, back, stomach, and joints) and tracked who developed depression over time. Here’s what stood out:
People with pain in five or more body areas had a 3.3 times higher risk of depression compared to those with no pain.
Even pain in a single area increased depression risk by about 44%.
The risk of depression grew steadily as more body areas were affected, showing a clear pattern.
Both acute (short-term) and chronic (long-term) pain raised depression risk, regardless of where the pain occurred.
The effects were especially strong in adults under 65 and in those with less education, highlighting the need for early intervention and support.
How Genetics & Inflammation Impact Pain
The study found that genetics play a role in why some people with widespread pain are more likely to develop depression. Using advanced genetic analysis, the researchers showed that having multiple pain sites can directly cause increased depression risk, not just correlate with it. Certain genes linked to widespread pain are also involved in brain regions that regulate emotion, which may help explain this connection.
Inflammation is another key piece of the puzzle. The researchers measured markers like C-reactive protein (CRP) and found that higher inflammation partly explained the link between pain and depression—especially when pain was widespread. About 15–29% of the pain-depression connection was mediated by inflammation markers. While this isn’t the whole story, it’s a significant piece that we can actually mitigate for in treatment (through lifestyle changes, therapy, diet, etc).
What Can We Control? Practical Takeaways for Patients with Pain
We can’t change our genetics, but we do have tools to address inflammation and support our mental health. Here’s how I guide my patients based on the latest research:
Diet: Anti-inflammatory foods—like leafy greens, berries, nuts, and fatty fish—can lower inflammation markers in the body. Remember, one person’s leafy green kale is another person’s food sensitivity and increased inflammation. Nutrition is not one-size-fits-all, and I encourage anyone exploring a health-supportive diet to meet with a holistic practitioner or nutritionist (call my office or email for our recommendation!).
Movement: Gentle exercise, even walking or stretching, helps reduce both pain and inflammation.
Mind-Body Practices: Meditation, breathwork, and mindfulness can regulate the nervous system and lower stress, which in turn may decrease inflammation.
Sleep: Prioritizing regular, restful sleep helps both pain and mood.
Social Support: Connection with others, whether through friends, family, or support groups, is protective against depression.
Professional Help: If you have pain in multiple areas or notice changes in your mood, early screening and intervention can make a real difference. Therapies like MORE and PRT (Pain Reprocessing Therapy) are also incredibly beneficial.
It’s important to remember that pain is not just a physical experience.
Addressing emotional and social factors is just as important as treating the body. This is the heart of the biopsychosocial model I use with my patients.
If you want to dive even deeper, I recommend viewing the whole study here.